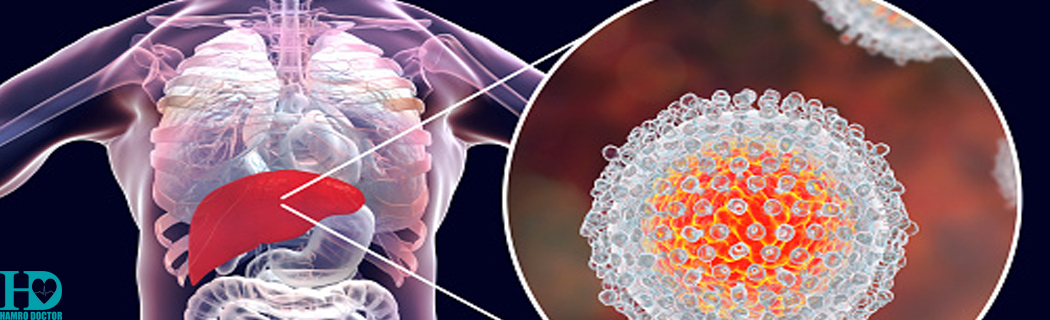
Hepatitis C is an infection caused by a virus that attacks the liver and leads to inflammation. Most people infected with the hepatitis C virus (HCV) have no symptoms. In fact, most people don't know they have the hepatitis C infection until liver damage shows up, decades later, during routine medical tests.
Hepatitis C is one of several hepatitis viruses and is generally considered to be among the most serious of these viruses. Hepatitis C is passed through contact with contaminated blood — most commonly through needles shared during illegal drug use.
Symptoms
Hepatitis C infection usually causes no symptoms until late in the course of chronic infection. In its earliest stages, beginning about one to three months after exposure to the virus, the following signs and symptoms occur in a small proportion of infected people:
- Fatigue
- Nausea or poor appetite
- Stomach pain
- Dark-colored urine
- Yellow discoloration in the skin and eyes (jaundice)
- Fever
- Muscle and joint pains
Signs and symptoms of chronic infection typically become evident after years and are the result of liver damage caused by the virus. These may initially include the symptoms of acute infection. Then, over time, signs and symptoms may include:
- Bleeding easily
- Bruising easily
- Itchy skin
- Fluid accumulation in your abdomen (ascites)
- Swelling in your legs
- Weight loss
- Confusion, drowsiness and slurred speech (hepatic encephalopathy)
- Spider-like blood vessels on your skin (spider angiomas)
When to see a doctor
Make an appointment with your doctor if you have any of the above signs and symptoms.
Causes
Hepatitis C infection is caused by the hepatitis C virus (HCV). HCV is spread when you come in contact with blood contaminated with the virus.
Diagnosis
Screening for hepatitis C
Testing for hepatitis C infection in people who have a high risk of coming in contact with the virus may help doctors begin treatment or recommend lifestyle changes that may slow liver damage. This is recommended because hepatitis C infection often begins damaging the liver before it causes signs and symptoms.
People who may want to talk to their doctors about screening for hepatitis C infection include:
- Anyone who has ever injected or inhaled illicit drugs
- Anyone with unexplained, unusual liver function test results
- Babies born to mothers with hepatitis C
- Health care and emergency workers who have been exposed to blood or accidental needle sticks
- People with hemophilia who were treated with clotting factors before 1987
- People who have ever undergone long-term hemodialysis treatments
- People who received blood transfusions or organ transplants before 1992
- Sexual partners of anyone diagnosed with hepatitis C infection
- People with HIV infection
- Anyone born from 1945 to 1965
- Anyone who has been in prison
Blood tests to diagnose hepatitis C
Blood tests may help to:
- Determine whether you have the hepatitis C virus
- Measure the quantity of the hepatitis C virus in your blood (viral load)
- Evaluate the genetic makeup of the virus (genotyping), which helps determine your treatment options
Testing samples of liver tissue to determine severity of liver damage
Your doctor may also recommend a procedure to remove a small sample of liver tissue for laboratory testing. A liver biopsy can help determine the severity of the disease and guide treatment decisions. During a liver biopsy, your doctor inserts a thin needle through your skin and into your liver to remove the tissue sample.
Preventions
Protect yourself from hepatitis C infection by taking the following precautions:
- Stop using illicit drugs. If you use illicit drugs, seek help.
- Be cautious about body piercing and tattooing. If you choose to undergo piercing or tattooing, look for a reputable shop. Ask questions beforehand about how the equipment is cleaned. Make sure the employees use sterile needles. If employees won't answer your questions, look for another shop.
- Practice safer sex. Don't engage in unprotected sex with multiple partners or with any partner whose health status is uncertain. Sexual transmission between monogamous couples may occur, but the risk is low.
Risk Factors
Your risk of hepatitis C infection is increased if you:
- Are a health care worker who has been exposed to infected blood, such as may happen if an infected needle pierces your skin
- Have ever injected or inhaled illicit drugs
- Have HIV
- Received a piercing or tattoo in an unclean environment using unsterile equipment
- Received a blood transfusion or organ transplant before 1992
- Received clotting factor concentrates before 1987
- Received hemodialysis treatments for a long period of time
- Were born to a woman with a hepatitis C infection
- Were ever in prison
- Were born between 1945 and 1965, the age group with the highest incidence of hepatitis C infection
Complications
Hepatitis C infection that continues over many years can cause significant complications, such as:
- Scarring of the liver tissue (cirrhosis). After 20 to 30 years of hepatitis C infection, cirrhosis may occur. Scarring in your liver makes it difficult for your liver to function.
- Liver cancer. A small number of people with hepatitis C infection may develop liver cancer.
- Liver failure. A liver that is severely damaged by hepatitis C may be unable to function adequately.
Treatment
Antiviral medications
Hepatitis C infection is treated with antiviral medications intended to clear the virus from your body. The goal of treatment is to have no hepatitis C virus detected in your body at least 12 weeks after you complete treatment.
Although medications to treat hepatitis C have been available for decades and have gradually improved with time, they have had serious side effects and required that a person be treated from 24 to 72 weeks. Side effects included depression, flu-like symptoms, and loss of healthy red or white blood cells (anemia or neutropenia). Therefore many people discontinued treatment.
Researchers have recently made significant advances in treatment for hepatitis C, combining new anti-viral medications with existing ones. As a result, people experience better outcomes, fewer side effects and shorter treatment times — some as short as 12 weeks. Regimens may vary depending on the hepatitis C genotype, presence of existing liver damage, other medical conditions and prior treatments, but they're generally much more effective today than previously.
Due to the pace of research, recommendations for medications and treatment regimens are changing rapidly, and treatment is also quite complex. It is therefore best to discuss your treatment options with a specialist.
Throughout treatment your doctor will monitor your response to medications.
Liver transplant
If your liver has been severely damaged, a liver transplant may be an option. During a liver transplant, the surgeon removes your damaged liver and replaces it with a healthy liver. Most transplanted livers come from deceased donors, though a small number come from living donors who donate a portion of their livers.
For people with hepatitis C infection, a liver transplant is not a cure. Treatment with antiviral medications usually continues after a liver transplant, since hepatitis C infection is likely to recur in the new liver.
Vaccinations
Although there is no vaccine for hepatitis C, your doctor will likely recommend that you receive vaccines against the hepatitis A and B viruses. These are separate viruses that also can cause liver damage and complicate treatment of hepatitis C.